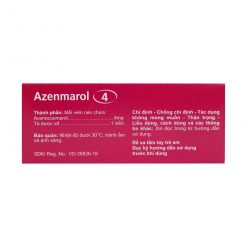
Chỉ định:
– Bệnh tim gây tắc mạch: Dự phòng biến chứng huyết khối tắc mạch do rung nhĩ, bệnh van hai lá, van nhân tạo.
– Nhồi máu cơ tim: Dự phòng biến chứng huyết khối tắc mạch trong nhồi máu cơ tim biến chứng như huyết khối trên thành tim, rối loạn chức năng thất trái nặng, loạn động thất trái gây tắc mạch khi điều trị tiếp thay cho heparin. Dự phòng tái phát nhồi máu cơ tim khi không dùng được aspirin.
– Điều trị huyết khối tĩnh mạch sâu và nghẽn mạch phổi và dự phòng tái phát khi thay thế tiếp cho heparin.
– Dự phòng huyết khối tĩnh mạch, nghẽn mạch phổi trong phẫu thuật khớp háng.
– Dự phòng huyết khối trong ống thông.
Liều dùng:
Liều lượng phải được điều chỉnh nhằm đạt mục đích ngăn cản cơ chế đông máu tới mức không xảy ra huyết khối nhưng tránh được chảy máu tự phát. Liều dùng tùy thuộc vào đáp ứng điều trị của từng người.
Liều uống thông thường: Trong ngày đầu là 4 mg/ngày, ngày thứ 2 là 4 – 8mg/ngày. Liều duy trì từ 1- 8mg/ ngày tùy theo đáp ứng sinh học. Việc điều chỉnh thường tiến hành từng nấc 1 mg.
Theo dõi sinh học và điều chỉnh liều:
Xét nghiệm sinh học thích hợp là đo thời gian prothrombin (PT) biểu thị bằng tỷ số chuẩn hóa quốc tế INR (International Normalized Ratio). Thời gian prothrombin cho phép thăm dò các yếu tố II, VII, X là những yếu tố bị giảm bởi thuốc kháng vitamin K. Yếu tố IX cũng bị giảm bởi thuốc kháng vitamin K, nhưng không được thăm dò bởi thời gian prothrombin.
INR là một cách biểu thị thời gian Quick có tính đến độ nhạy của thuốc thử (thromboplastin) dùng để làm xét nghiệm, nên giảm được những thay đổi thất thường giữa các labo.
Khi không dùng thuốc kháng vitamin K, INR ở người bình thường là 1. Khi dùng thuốc trong những tình huống dưới đây, trong đa số trường hợp đích INR cần đạt là 2,5, dao động trong khoảng 2 và 3. INR dưới 2 phản ánh dùng thuốc chống đông máu chưa đủ. INR trên 3 là dùng thừa thuốc. INR trên 5 là có nguy cơ chảy máu.
Nhịp độ kiểm tra sinh học: Lần kiểm tra đầu tiên tiến hành 48 giờ ± 12 giờ sau lần uống thuốc kháng vitamin K đầu tiên để phát hiện sự tăng nhạy cảm của cá nhân. Nếu INR trên 2, báo hiệu sẽ quá liều khi cân bằng, vì vậy phải giảm bớt liều. Những lần kiểm tra sau tiến hành hàng ngày hoặc cách nhật cho tới khi INR ổn định, sau đó cách xa dần tùy theo đáp ứng, dài nhất là 12 tuần một lần. Cân bằng điều trị đôi khi chỉ đạt sau nhiều tuần. Sau mỗi lần thay đổi liều, phải kiểm tra INR 1 – 2 ngày sau đó và nhắc lại cho tới khi đạt ổn định.
Nhìn chung, INR từ 2 – 3 được khuyến cáo để phòng hoặc điều trị huyết khối tắc tĩnh mạch, bao gồm nghẽn mạch phổi, rung nhĩ, bệnh van tim, hoặc van sinh học. INR từ 2,5 đến 3,5 được khuyến cáo sau nhồi máu cơ tim, người bệnh van tim cơ học, hoặc ở một số người bệnh có huyết khối hoặc hội chứng kháng phospholipid. INR cao hơn có thể được khuyến cáo cho tắc mạch tái phát.
Liều ở người cao tuổi: Liều khởi đầu phải thấp hơn liều người lớn. Liều trung bình cân bằng trong điều trị thường chỉ bằng 1/2 tới 3/4 liều người lớn.
Điều trị nối tiếp heparin-liệu pháp: Do tác dụng chống đông máu chậm của các thuốc kháng vitamin K, nên heparin phải được duy trì với liều không đổi trong suốt thời gian cần thiết, nghĩa là cho tới khi INR nằm trong trị số mong muốn 2 ngày liên tiếp. Trong trường hợp có giảm tiểu cầu do heparin, không nên cho kháng vitamin K sớm ngay sau khi ngừng heparin vì có nguy cơ tăng đông máu do protein S (chống đông máu) bị giảm sớm. Chỉ cho kháng vitamin K sau khi đã cho các thuốc kháng thrombin (danaparoid hoặc hirudin).
Cần dừng thuốc chống đông máu 5 ngày trước khi phẫu thuật. Nếu ngày trước khi phẫu thuật INR ≥ 1,5 thì cần cho uống vitamin K dạng tiêm 1 – 5mg. Nếu cầm máu tốt thì có thể cho dùng lại thuốc (acenocoumarol) với liều duy trì bình thường vào tối ngày phẫu thuật hoặc sáng hôm sau.
Bệnh nhân dừng thuốc trước khi phẫu thuật được coi là có nguy cơ huyết khối cao nên có thể cần hỗ trợ bằng một loại heparin phân tử lượng thấp (dùng với liều điều trị). Cần dừng heparin phân tử lượng thấp ít nhất 24 giờ trước khi phẫu thuật. Nếu phẫu thuật có nguy cơ chảy máu cao, không được dùng lại heparin phân tử lượng thấp trong vòng ít nhất 48 giờ sau phẫu thuật.
Bệnh nhân đang dùng thuốc (acenocoumarol) cần phẫu thuật gấp mà có thể chậm lại khoảng 6 – 12 giờ thì có thể cho tiêm tĩnh mạch 5 mg vitamin K để đảo ngược tác dụng chống đông. Nếu không thể trì hoãn thì phải cho dùng cả vitamin K tiêm và hỗn hợp prothrombin khô (ví dụ 25 đơn vị/kg) và phải xét nghiệm xác định INR trước khi phẫu thuật.
Cách dùng:
Acenocoumarol thường được uống một lần vào cùng một thời điểm mỗi ngày.
Chống chỉ định:
Mẫn cảm đã biết với các dẫn chất coumarin hay với bất cứ thành phần nào của thuốc.
Thiếu hụt vitamin C, viêm màng trong tim do vi khuẩn, loạn sản máu hoặc bất kỳ rối loạn máu nào có tăng nguy cơ xuất huyết.
Tăng huyết áp (nặng).
Suy gan nặng, đặc biệt khi thời gian prothrombin đã bị kéo dài.
Nguy cơ chảy máu, mới can thiệp ngoại khoa về thần kinh và mắt hay khả năng phải mổ lại.
Tai biến mạch máu não (trừ trường hợp nghẽn mạch ở nơi khác).
Suy thận nặng (Clcr < 20 ml/phút).
Giãn tĩnh mạch thực quản.
Loét dạ dày – tá tràng đang tiến triển.
Không được phối hợp với aspirin liều cao, thuốc chống viêm không steroid nhân pyrazol, miconazol dùng đường toàn thân, âm đạo; phenylbutazol, cloramphenicol, diflunisal.
Không dùng acenocoumarol trong vòng 48 giờ sau khi sinh.
Các trường hợp thận trọng khi dùng thuốc:
Các tình trạng cần thận trọng:
– Phải lưu ý đến khả năng nhận thức của người bệnh trong quá trình điều trị (nguy cơ uống thuốc nhầm). Hướng dẫn cẩn thận để họ tuân thủ chỉ định chính xác, hiểu rõ nguy cơ và thái độ xử lý, nhất là với người cao tuổi.
– Phải nhấn mạnh việc uống thuốc đều hàng ngày vào cùng một thời điểm.
– Phải xét nghiệm kiểm tra tỷ số chuẩn hóa quốc tế (INR) định kỳ và tại cùng một nơi.
– Trường hợp can thiệp ngoại khoa, phải xem xét từng trường hợp để điều chỉnh hoặc tạm ngừng dùng thuốc chống đông máu, căn cứ vào nguy cơ huyết khối của người bệnh và nguy cơ chảy máu liên quan đến từng loại phẫu thuật.
– Theo dõi cẩn thận và điều chỉnh liều cho phù hợp ở người suy thận vừa và nhẹ hoặc hạ protein máu.
– Tai biến xuất huyết dễ xảy ra trong những tháng đầu điều trị nên cần theo dõi chặt chẽ, đặc biệt khi người bệnh ra viện trở về nhà.
– Không nên dừng thuốc đột ngột.
- Thành phần tá dược của thuốc này có lactose vì vậy không nên dùng thuốc này cho bệnh nhân bị di truyền không dung nạp galactose, bị thiếu hụt lactase hoặc kém hấp thu glucose-galactose.
Các khuyến cáo dùng thuốc cho phụ nữ có thai và cho con bú:
Thời kỳ mang thai:
Đã có thống kê khoảng 4% dị dạng thai nhi khi người mẹ dùng thuốc này trong quý đầu thai kỳ. Vào các quý sau, vẫn thấy có nguy cơ (cả sảy thai). Vì vậy tránh dùng cho phụ nữ có thai, đặc biệt là trong 3 tháng đầu và 3 tháng cuối thai kỳ. Chỉ dùng thuốc khi không thể cho heparin.
Thời kỳ cho con bú:
Tránh cho con bú. Nếu phải cho bú thì nên bù vitamin K cho đứa trẻ.
Tác động của thuốc đến khả năng lái xe và vận hành máy móc:
Thuốc không gây ảnh hưởng đến khả năng lái xe hay vận hành máy móc.
Tương tác của thuốc với các thuốc khác và các loại tương tác khác:
Rất nhiều thuốc có thể tương tác với thuốc kháng vitamin K nên cần theo dõi người bệnh 3 – 4 ngày sau khi thêm hay bớt thuốc phối hợp.
Chống chỉ định phối hợp
– Aspirin (nhất là với liều cao trên 3g/ngày) làm tăng tác dụng chống đông máu và nguy cơ chảy máu do ức chế ngưng tập tiểu cầu và chuyển dịch thuốc uống chống đông máu ra khỏi liên kết với protein huyết tương.
– Miconazol: Xuất huyết bất ngờ có thể nặng do tăng dạng tự do trong máu và ức chế chuyển hoá của thuốc kháng vitamin K.
– Phenylbutazon làm tăng tác dụng chống đông máu kết hợp với kích ứng niêm mạc đường tiêu hoá.
– Thuốc chống viêm không steroid nhóm pyrazol: Tăng nguy cơ chảy máu do ức chế tiểu cầu và kích ứng niêm mạc đường tiêu hóa.
Không nên phối hợp:
– Aspirin với liều dưới 3 g/ngày.
– Các thuốc chống viêm không steroid, kể cả loại ức chế chọn lọc COX-2
– Cloramphenicol: Tăng tác dụng của thuốc uống chống đông máu do làm giảm chuyển hoá thuốc này tại gan. Nếu không thể tránh phối hợp thì phải kiểm tra INR thường xuyên hơn, hiệu chỉnh liều trong và sau 8 ngày ngừng cloramphenicol.
– Diflunisal: Tăng tác dụng của thuốc uống chống đông máu do cạnh tranh liên kết với protein huyết tương. Nên dùng thuốc giảm đau khác, ví dụ paracetamol.
Thận trọng khi phối hợp:
Alopurinol, aminoglutethimid, amiodaron, androgen, thuốc chống trầm cảm cường serotonin, benzbromaron, bosentan, carbamazepin, cephalosporin, cimetidin (trên 800 mg/ngày), cisaprid, cholestyramin, corticoid (trừ hydrocortison dùng điều trị thay thế trong bệnh Addison), cyclin, thuốc gây độc tế bào, fibrat, các azol trị nấm, fluoroquinolon, các loại heparin, nội tiết tố tuyến giáp, thuốc gây cảm ứng enzym, các statin, macrolid (trừ spiramycin), neviparin, efavirenz, nhóm imidazol, orlistat, pentoxifyllin, phenytoin, propafenon, ritonavir, lopinavir, một số sulfamid (sulfamethoxazol, sulfafurazol, sulfamethizol), sucralfat, thuốc trị ung thư (tamoxifen, raloxifen), tibolon, vitamin E trên 500 mg/ngày, rượu, thuốc chống kết tập tiểu cầu, thuốc tiêu huyết khối,…cũng làm thay đổi tác dụng chống đông máu.
Tác dụng không mong muốn:
Các biểu hiện chảy máu là biến chứng hay gặp nhất, có thể xảy ra trên khắp cơ thể: Hệ thần kinh trung ương, các chi, các phủ tạng, trong ổ bụng, trong nhãn cầu,….
Đôi khi xảy ra tiêu chảy (có thể kèm theo phân nhiễm mỡ), đau khớp riêng lẻ.
Hiếm khi xảy ra: Rụng tóc; hoại tử da khu trú, có thể do di truyền thiếu protein C hay đồng yếu tố là protein S; mẩn da dị ứng.
Rất hiếm thấy bị viêm mạch máu, tổn thương gan.
Hướng dẫn cách xử trí ADR
Xem mục Quá liều và cách xử trí.
Quá liều và cách xử trí:
Triệu chứng:
Biểu hiện nổi bật của quá liều là xuất huyết, có thể xảy ra trong vòng 1 – 5 ngày sau khi uống thuốc. Các biểu hiện xuất huyết có thể nhận thấy : Mũi chảy máu, nôn ra máu, ho ra máu, xuất huyết dạ dày – ruột, xuất huyết âm đạo, đái ra máu (với cơn đau quặn thận), xuất huyết dưới da, chảy máu nướu, tụ máu, và chảy máu trong khớp hay rong kinh.
Có thể thấy triệu chứng nhịp tim nhanh, hạ huyết áp, rối loạn tuần hoàn ngoại vi do mất máu, buồn nôn, nôn mửa, tiêu chảy và đau bụng.
Xử trí:
Xử trí quá liều thường căn cứ vào INR và các dấu hiệu chảy máu, các biện pháp điều chỉnh phải tuần tự để không gây nguy cơ huyết khối. Nếu đã dùng thuốc chống đông nhưng không dùng vitamin K, cần xét nghiệm lại INR 2 – 3 ngày sau để đảm bảo rằng INR đã xuống.
-Nếu INR < 5, ở mức điều trị, người bệnh không có biểu hiện chảy máu hoặc không cần hiệu chỉnh nhanh đông máu trước phẫu thuật: Bỏ 1 lần uống thuốc, rồi lại tiếp tục điều trị với liều thấp hơn khi đã đạt INR mong muốn. Nếu INR rất gần với INR mong muốn, thì giảm liều mà không cần phải bỏ lần uống thuốc.
-Nếu 5 < INR < 8, không có biểu hiện chảy máu khác ngoài chảy máu lợi hoặc chảy máu cam: Bỏ 1 hoặc 2 lần uống thuốc chống đông máu, đo INR thường xuyên hơn rồi khi đã đạt INR mong muốn, uống lại thuốc với liều thấp hơn.
-Nếu 5 < INR < 8, có chảy máu nhẹ: Ngừng thuốc, cho dùng vitamin K từ 1 – 3 mg theo đường truyền tĩnh mạch chậm. Chỉ dùng lại acenocoumarol khi INR < 5,0.
-Nếu INR > 8, không có chảy máu: Ngừng acenocoumarol, dùng 1 – 5 mg phytomenadion (vitamin K1) (sử dụng dạng thuốc tiêm thay cho đường uống). Sau 24 giờ nếu INR vẫn cao thì lặp lại điều trị với vitamin K. Chỉ dùng lại acenocoumarol khi INR < 5,0.
-Nếu INR > 8, chảy máu nhẹ: Ngừng thuốc, cho dùng vitamin K từ 1 – 3 mg theo đường tiêm tĩnh mạch chậm. Sau 24 giờ nếu INR vẫn cao thì lặp lại liều vitamin K. Chỉ dùng lại acenocoumarol khi INR < 5,0.
– Trong trường hợp có biểu hiện chảy máu nặng hoặc quá liều nặng (ví dụ INR > 20): Ngừng thuốc, tiêm tĩnh mạch chậm 5 mg vitamin K, cho dùng hỗn hợp prothrombin khô ( yếu tố II, VII, IX và X) 25 – 50 đơn vị/kg (nếu không có hỗn hợp prothrombin khô thì thay thế bằng huyết tương tươi đông lạnh 15 ml/kg nhưng hiệu quả sẽ kém hơn). Không nên dùng kèm yếu tố VIIa trong trường hợp cấp cứu đảo ngược tác dụng chống đông.
Trường hợp ngộ độc do tai nạn, thì cũng phải đánh giá theo INR và biểu hiện biến chứng chảy máu. Phải đo INR nhiều ngày sau đó (2-5 ngày), có tính đến nửa đời kéo dài của thuốc chống đông máu. Dùng vitamin K để hiệu chỉnh tác dụng của thuốc chống đông máu.
Các đặc tính dược lực học:
Acenocoumarol là một dẫn chất coumarin kháng vitamin K. Những thuốc này ức chế enzym vitamin K epoxid reductase, dẫn tới ngăn cản quá trình chuyển acid glutamic thành acid gamma-carboxyglutamic của các protein tiền thân của các yếu tố đông máu II, VII, IX, X.
Như vậy là các dẫn chất coumarin kháng vitamin K có tác dụng chống đông máu gián tiếp bằng cách ngăn cản sự tổng hợp các dạng hoạt động của các yếu tố đông máu trên (II, VII, IX, X).
Sau khi uống acenocoumarol, tác dụng đối với thời gian prothrombin kéo dài thường đạt tối đa trong vòng từ 24 đến 48 giờ, tùy thuộc liều dùng. Sau khi ngừng thuốc 48 giờ, thời gian prothrombin trở về mức trước khi dùng thuốc.
Sau khi uống, nói chung, các dẫn chất coumarin kháng vitamin K gây hạ prothrombin máu trong vòng 36 đến 72 giờ. Cân bằng điều trị bằng thuốc kháng vitamin K đòi hỏi nhiều ngày. Sau khi ngừng thuốc, tác dụng chống đông máu còn có thể kéo dài thêm 2 – 3 ngày. Thuốc có thể hạn chế được sự phát triển của các cục huyết khối đã có trước và ngăn ngừa được các triệu chứng huyết khối tắc mạch thứ phát, tuy không có tác dụng tiêu huyết khối trực tiếp vì không đảo ngược được thương tổn của mô bị thiếu máu cục bộ.
So với wafarin và phenprocoumon, acenocoumarol có lợi thế là thời gian tác dụng ngắn hơn.
Các đặc tính dược động học:
Acenocoumarol được hấp thu nhanh qua đường tiêu hoá. Sinh khả dụng đường uống đạt 60%. Một phần đáng kể đồng phân S(-)-acenocoumarol qua chuyển hóa bước đầu tại gan, trong khi sinh khả dụng của đồng phân R(+)-acenocoumarol là 100%. Thuốc gắn mạnh với protein huyết tương (99%). Nồng độ đỉnh của thuốc trong huyết tương đạt trong vòng 1 – 3 giờ. Thể tích phân bố 0,16 – 0,34 lít/kg. Acenocoumarol qua nhau thai và một phần nhỏ được phát hiện trong sữa mẹ.
Acenocoumarol bị chuyển hóa ở gan bởi hệ enzym cytochrom P450 (isoenzym CYP2C9 chuyển hóa đồng phân S, đồng phân R bị chuyển hóa bởi một số isoenzym khác) thành các chất chuyển hóa amin và acetamid không có hoạt tính. Một vài chất chuyển hóa khác như diastereoisometric alcohol và chất chuyển hóa hydroxyl có thể có hoạt tính. Các nhà lâm sàng cần biết khả năng một số người bệnh nhạy cảm cao với acenocoumarol do tính đa hình của ty lạp thể ở gan, và có thể phải giảm liều ở người bệnh đó.
Nửa đời thải trừ của acenocoumarol khoảng 8 -11 giờ.
Thuốc đào thải chủ yếu qua nước tiểu (60% trong khoảng 1 tuần) ở dưới dạng chuyển hoá và một phần qua phân(29% trong khoảng 1 tuần).


 English
English